Chemotherapy gowns: Why your healthcare facilities should not compromise on quality for price
Your nurses and infection prevention staff that care for patients receiving chemotherapy are potentially at risk from exposure to the hazardous drugs (HDs) they must help deliver. This article touches upon the risks to staff from this exposure, and lays out the reasons why personal protective equipment (PPE), particularly chemotherapy gowns, are essential to protecting staff.
Jordan Rosenfeld
Essential Insights contributor, healthcare writer
What is a hazardous drug?
According to the “Safe Handling Toolkit” by the Oncology Nursing Society (ONS), a drug meets the criteria of being hazardous if it has:1
- Carcinogenicity
- Teratogenicity or other developmental toxicity
- Reproductive toxicity
- Organ toxicity at low doses
- Genotoxicity
- Structure and toxicity profiles of new drugs that mimic existing drugs determined hazardous by the above criteria
More than half of hazardous drugs are antineoplastic agents used in cancer treatment2 and are among the most toxic administered in your healthcare settings.3
Effects of exposure to hazardous drugs
Acute and chronic effects of healthcare professional exposure to hazardous drugs
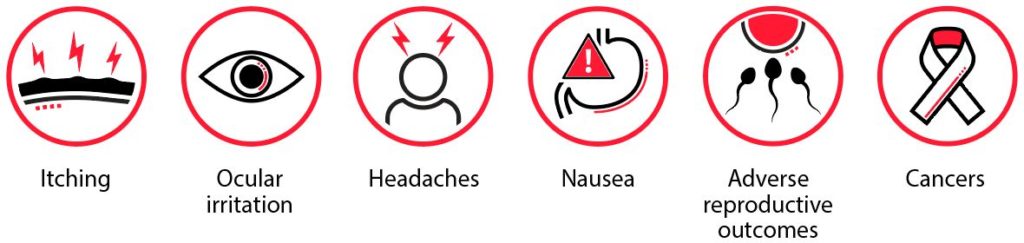
Your oncology nurses and infection prevention staff are exposed in the workplace to HDs that can cause acute and chronic health effects, such as: skin rashes, ocular irritation, headaches, nausea and vomiting, adverse reproductive outcomes (including infertility, spontaneous abortions, and congenital malformations), and cancers, including leukemia and others.4
While the benefts of hazardous drug exposure outweigh the risks for patients, there are no benefts for your healthcare workers.

The costs/risks of chemotherapy exposure to your staff
According to an ONS publication, “Safe Handling of Hazardous Drugs,” widespread environmental contamination with HDs has been frequently reported, placing healthcare workers at risk.5
Additionally, body fuids of patients who have received a HD within 48 hours also pose a risk to your healthcare workers, as drug traces have been found in body fuids within this time frame.6
Most healthcare worker exposure to these drugs come through absorption of the drugs through contact with skin or mucous membranes, though inadvertent inhalation or injection can occur as well.
Wearing a lab coat (instead of a chemotherapy gown) is not enough protection against adverse effects of HDs, and could lead to cross contamination of other surfaces and other staff. Chemotherapy gowns are the recommended PPE to handle HDs, according to ONS.1
PPE, including chemo tested gowns and gloves, need to be worn when administering treatment, and also when in contact with body fuids of patients within 48 hours of drug administration.4 Other measures to protect your staff against HDs include biosafety cabinets, aseptic containment isolators, and engineering controls related to the rooms where HDs are stored, such as ventilation and temperature controls.5
Body fuids of patients who have received
a HD within 48 hours also pose a risk to healthcare workers, as drug traces have been found in body fuids within this time frame6.
Other statistics/risks
At this time, there is no reliable method for biologic monitoring of occupational exposure to HDs, reinforcing the importance of effective PPE to protect your healthcare workers.5
Why facilities should use a premium gown
Because of the serious nature of exposure to HDs, chemotherapy gowns are worth the price to protect staff and hospitals or health facilities. Chemotherapy gowns must meet the following criteria, according to ONS:1
- Disposable, lint free, and rated to resist chemotherapy permeation
- Should have long sleeves and elastic or knit cuffs, fasten in the back (no open front), and be without seams or closures that could allow HD exposure
- Polyethylene-coated polypropylene or other laminate is recommended
- They must meet USP <800> standards for handling hazardous drugs. (The United States Pharmacopeial Convention is a nonproft organization that sets standards around the quality and safety of medications.)
Additionally, cloth laboratory coats, scrubs, or coveralls should not be worn in place of chemotherapy gowns.
To ensure safe use of these gowns, your staff should only wear these gowns during patient care and interaction, or during activities that require protection, such as transportation, preparation, post-treatment care, and disposal, to ensure they are used safely. Your staff should also inspect for visible defects such as flaws or tears before wearing them, and change gowns after a spill, splash, or 2-3 hours of continuous use.
Cardinal Health™ ChemoPlus™ Chemotherapy Gowns
Cardinal Health recently launched a new chemotherapy gowns and sleeves portfolio.
The ChemoPlus™ Chemotherapy Gowns and Sleeves provide AAMI Level 3 fuid protection and a barrier against HDs.
The ChemoPlus™ Chemotherapy Gowns and Sleeves provide AAMI Level 3 fuid protection and a barrier against HDs. They are designed with reinforced critical zones — chest, sleeve seam, front belt attachment points — the places where infectious material is most likely to come into contact with the wearer. ChemoPlus™ Gowns and Sleeves are manufactured in North America, at Cardinal Health-owned facilities, with raw materials mostly sourced within the United States.7
The gown has been evaluated for resistance to permeation of 16 chemotherapy drugs per ASTM F739-20.8 These AAMI Level 3 gowns and sleeves are designed to meet the strictest standards for moderate fuid protection. They also meet USP <800> standards for handling HDs and have FDA 510(k) clearance.
The gown has been evaluated for resistance to permeation of 16 chemotherapy drugs per ASTM F739-20.


Conclusion
The cost of a premium chemotherapy gown is worth the protection it offers against harm that can be caused to your staff by exposure to HDs.
Sources
1.https://www.ons.org/sites/default/fles/2018-06/ONS_Safe_Handling_Toolkit_0.pdf 2. Denise Menonna-Quinn, “Evaluating usage among inpatient and outpatient oncology nurses” 3. AnnMarie Lee Walton, “Surface Contamination With Antineoplastic Drugs on Two Inpatient Oncology Units” 4. https://www.cdc.gov/niosh/topics/hazdrug/default.html 5. “Safe Handling of Hazardous Drugs,” Oncology Nursing Society. PDF 6. https://voice.ons.org/news-and-views/what-are-onss-recommendations-for-gowns-when-handling-hazardous-drugs 7. “Chemo Protection That Works As Hard As You Do.” Cardinal Health. PDF 8. ASTM International. Standard Test Method for Permeation of Liquids and Gases Through Protective Clothing Materials Under Conditions of Continuous Contact. https://www.astm.org/Standards/F739.htm. Accessed October 6, 2021

