The Importance of
Proper Injection
Technique in
Insulin Delivery
In a recent Canadian study1 all self-injecting patients (surveyed in the home setting) made at least one injection technique error, indicating the need for ongoing training and education on proper injection technique. It’s important to review these techniques on a regular basis especially with patients managing diabetes.
Download a copy of our injection technique checklist.
Care settings should follow best practice recommendations on the safe use of injection devices. Wherever diabetes care is being delivered, it is the responsibility of the Health Care Provider (HCP) and the care setting to ensure that policy and procedures are being followed to promote the safest environment for anyone exposed to the potential for a needlestick injury. Research has repeatedly shown that risk assessment, ongoing education and continuous quality improvement programs contribute to the development and sustainability of this “safe culture”.2,4,7
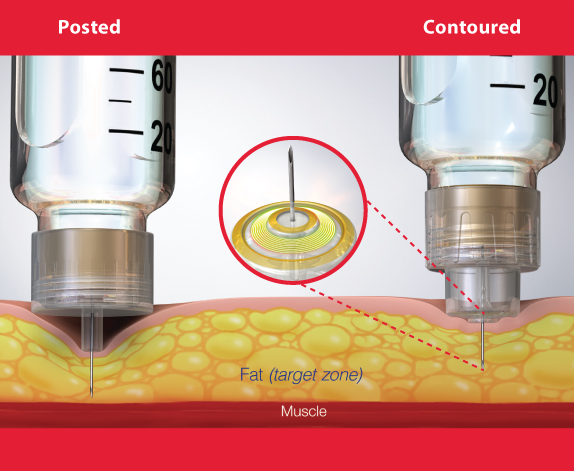
Two components of a safe injection for the patient involves delivering an accurate dose of medication into the appropriate tissue.5, 10 To accomplish this, the HCP must choose the appropriate device and use it safely with the correct technique to deliver the medication into the subcutaneous tissue.6,13,16 All HCPs should be trained in the use of the Safety engineered device.3,8,15,30 HCPs should use the shortest possible length of a safety engineered device for the pen or syringe to avoid using a skin lift and ensure delivery into the subcutaneous tissue.22,38,39 Where pen devices are used there must be an enforced policy of one pen per patient.9,14,17
SED pen needles should have protection from exposure at both ends of the needle to prevent NSI before and after use.3,15,18,20,21 All SEDs being used should have the following features:
• an easy one hand activation;
• a clear view of the tip of the sharp at the entry site;
• a clear indication of the dose delivery;
• a clear indication of the activation of the safety feature; and
• no exposure to the sharp following the dose administration.2,4,11,12,15
Featured Products
BD AutoShield Duo™ Safety Pen Needles
- Reduces the risk of medication error and improves dose accuracy
- Automatic dual-protection shields enable reliable insulin delivery

BD Nano™ PRO, Ultra-Fine™ Pen Needles
- Provides a more reliable injection depth for insulin delivery
- Compatible with leading GLP-1 and insulin pens in Canada
LinkedIn Sources:
* Rini C, et al. J Diabetes Sci Technol. 2019;13(3):533-545.
** Hirsch L, et al. Diabetes Technol Ther. 2014;16(12):867-873
Article Sources:
1. Bari B, et al. Diabetes Ther. 2020;11:2595-2609 2. Fit safety (2018) FIT4Diabetes. Available at: http://www.fit4diabetes.com/canada-english/fit-safety-recomendations/ (Accessed: November 9, 2022).
2. Adam D. Needlestick and sharps injuries: practice update. Nursing Standard 2012; 26:49-57.
3. Adams D. To the point: needlestick injuries, risks, prevention and the law. British Journal of Nursing 2011; 20:3356-3359.
4. Adams D, Elliott T. Impact of safety needle devices on occupationally acquired needle stick injuries: a four year prospective study. Journal of Hospital Infection 2006; 64:50-55.
5. American Association of Diabetes Educators. Insulin self-administration instruction: use of engineered sharps injury protection devices to meet OSHA regulations. The Diabetes Educator 2002; 28:730-734.
6. Annersten M, Willman A. Performing subcutaneous injections: a literature review. Worldviews Evidenced Based Nursing 2005; 2:122-130.
7. Bi P, Tullt P, Pearce S, Hiller J. Occupational blood and body fluid exposure in an Australian teaching hospital. Epidemiology and Infection 2006; 134:465-471.
8. Canadian Centre for Occupational Health and Safety, OSH answers, Needlestick injuries, http://www.ccohs.ca/oshanswers/diseases/needlestick_injuries.html Accessed May 12, 2012.
9. CDC. Clinical Reminder: Insulin pens must never be used for more than one person.www.cdc.gov/injectionsafety/clinicalreminders/insulin-pens.html. Accessed
June 12, 2012.
10. FIT: Forum for injection technique in Canada: recommendations for best practice in injection technique. 2011. www.bd.com/resource.aspx?IDX=
11. Jagger J, Perry J. Power in numbers: using EPINet data to promote protective policies for healthcare workers. Journal of Infusion Nursing 2002; 25:6S s15-20.
12. Kiss P, De Meester M., Braeckman, L.Needlestick injuries in nursing homes: the prominent role of insulin pens. Infection Control and Hospital Epidemiology December 2008; 29(12):1192-1194.
13. Lamontagne F, Abiteboul D, Lolom I, Pellissier G, Tarantola A, Descamps J, Bouvet E. Role of safety-engineered devices in preventing needlestick injuries in 32 French hospitals. Infection Control 2007; 28:18-23.
14. Le Floch JP, Herbreteau C, Lange F, Perlmuter L. Biologic material in needles and cartridges after insulin injection with a pen in diabetic patients. Diabetes Care 1998; 9:1502-1504.
15. Ontario Nurses’ Association. Health and safety hazards: needle/sharp safety. www.ona.org/health_safety/hazards/needle_sharps_safety.html – accessed June 1, 2012.
16. OSHA, US department of labour http://www.osha.gov/pls/oshaweb/owadisp.show_document?p_table=STANDARDS&p_id=10051 accessed May 28, 2012.
17. Pellissier G, Migueres B, Taranatola A, Abiteboul D, Lolum I, Bouvet E. GERES Group. Risk of needlestick injuries by injection pens. Journal of Hospital Infections 2006; 63:60-64.
18. Strauss K, WISE Consensus Group. WISE recommendations to endure the safety of injection in diabetes. Diabetes & Metabolism 2012; 38:S9-S14.
19. Strauss K, Hannet I, McGonigle J, Parkes J, Ginsberg B, Jamal R, Frid F. Ultrashort (5mm) insulin needles:trial results and clinical recommendation. Practical Diabetes International 1999; 6:22-25.
20. Trim J. A review of needle-protective devices to prevent sharps injuries. British Journal of Nursing 2004; 13(3)144-153.
21. Trim J, Elliott T. A review of sharps injuries and preventative strategies. Journal of Hospital Infection 2003;53:237-242.

