DVT Debunked: Why DVT prevention is important to clinical staff
The Smart Compression™ Educates DVT Debunked series introduces several common misconceptions – or myths – about blood clot prevention and provides resources and evidence to clarify and educate.
Patricia Chaney
Essential Insights contributor, healthcare writer
Myth:
Deep vein thrombosis (DVT) prevention is not a priority for clinical staff.
Truth:
Venous thromboembolism (VTE), which includes DVT and pulmonary embolism (PE), is the leading cause of preventable death in hospitalized patients. Many cases occur in outpatient settings but are related to recent surgery or hospitalization. Clinical staff may not always see the effects, yet prevention begins in the hospital. Clinical staff are vital at preventing VTE in the hospital and educating patients on at-home prevention.
Nurses, providers and caregivers on the front lines feel the strain of numerous competing priorities, and many are fighting burnout from the pandemic. But, with a few steps, you can prioritize VTE prevention and aim to make it a rare event.
Why it matters
Julia Shelton, DNP, APRN, CNS, shared a story from her hospital, where a new mom was found dead during hourly rounding after having a scheduled C-section. “We did find out eventually she did have a PE,” Shelton said. “We are so close to the patients we serve. … it has heightened our awareness that PEs do happen. We do have the opportunity to prevent them.”
In the United States, about 540,000 hospitalized patients develop a VTE every year. Up to 70% of hospital-associated VTE cases can be prevented with appropriate interventions.
It’s important to begin prevention in the hospital, because DVT and PE can lead to long-term complications for patients. Patients who develop DVT are more likely to develop blood clots again later in life. Some may develop post-thrombotic syndrome, which affects their quality of life.
Signs and symptoms
DVT is a blood clot that occurs in one of the deep veins in the body, most often in the legs. If the blood clot in a vein breaks loose, it can travel through the bloodstream and lodge in an artery in the lungs. This blocks the blood flow to the lung and leads to a PE.
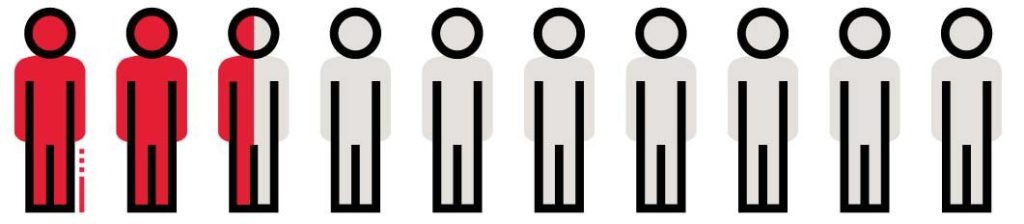
DVT often has few symptoms, which means clinical staff need to be proactive with prevention. For about 25% of people with PE, the first symptom is sudden death.
For about 25%
of people with PE, the first symptom is sudden death1.
Other symptoms of DVT include2:
Importance of prevention and treatment
About 50% of patients are poorly prophylaxed. Risk assessment tools and guidelines are available to categorize patients based on risk and choose appropriate prophylaxis, such as anticoagulation, mechanical compression, or compression stockings.
Prevention begins in the hospital or surgical center, but it also continues at home. More surgeries are moving to outpatient procedures. More than half of blood clots that occur in an outpatient setting, occur after a recent surgery or hospitalization, making education in a healthcare facility that much more important.
Role of clinical staff
Clinical staff are at the front lines of prescribing VTE prophylaxis and encouraging patients to use it effectively. They’re also there to educate patients on the importance of using compression therapy properly.
Risk assessment tools and a proactive approach toward VTE prevention makes it easier to implement and encourage patient use.
Education by staff to establish good habits before discharge is important to preventing DVT and readmissions. Although these are stressful times with competing priorities, when clinical staff take these steps toward prevention, patients experience the benefits.
